This is an online e log book to discuss our patient de-identified health data shared after taking his / her / guardians signed informed consent. Here we discuss our individual patients problems through series of inputs from available global online community of experts with an aim to solve those patients clinical problem with collective current best evident based input.
This E blog also reflects my patient centered online learning portfolio and your valuable inputs on the comment box is welcome
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan
This is an updated blog taking references from:
https://nvprathyusha100.blogspot.com/2023/11/48-yr-male-with-ascites-pedal-edema.html
https://chitlaswagathrollno31.blogspot.com/2023/12/39-yr-old-male-with-abdominal.html
39 yr old male cab driver by occupation resident of west bengal came to opd with chief complaints of
CHIEF COMPLAINTS:
1.Abdominal distension since 2 months
2.Bilateral pedal edema since 2 months
3.decreased appetite since 2 months
4.decreased urine output since 1 month
HISTORY OF PRESENTING ILLNESS:
Patient was apparently asymptomatic 2 months back then he developed abdominal distension which is insidious in onset gradually progressive associated with decreased appetite and he observed bilateral pedal edema upto knees since 2 months which is of pitting type which increased on walking and relieved with rest.Decreased urine output since 1 month which is insidious in onset and gradually progressive
No h/o fever, cough, breathlessness.
PAST HISTORY:
Not a k/c/o DM,Asthma,TB, Epilepsy, Thyroid disorders ,HTN,CKD,CVA,CAD
PERSONAL HISTORY:
Diet :Mixed
Appetite : normal
Sleep: adequate
Bowel and bladder movements: regular
Occassional Alcoholic (180ml weekly once) - stopped 1 yr back
Smokes Beedi 1pack/day --stopped 3months back
GENERAL EXAMINATION:
Patient is conscious,coherent and cooperative
Moderately built and nourished
No Pallor, icterus, cyanosis , clubbing, Lymphadenopathy
Bilateral pedal edema pitting type
VITALS:
PR : 86 bpm
BP : 110/80 mmHg
RR : 20 CPM
Temperature : 98.4f
Spo2 : 98 % on RA
Abdominal girth:86cms
Weight:46kg
On The day of presentation
SYSTEMIC EXAMINATION:
ABDOMINAL EXAMINATION:
Inspection:
Shape - distended
Flanks-full
Umbilicus - inverted
All quadrants moves equally with respiration
No engorged veins, visible pulsations,scars,sinuses
Palpation:
All inspectory findings are confirmed
No local rise of temperature
Abdomen is soft and non tender
spleen and liver -not palpable
No other palpable masses
Hernial orifice are free
Percussion:
Shifting dullness present
Fluid thrill present
Auscultation:
Bowel sounds heard.
CVS EXAMINATION:
Jvp not raised
Inspection:
Shape of chest - elliptical
No visible pulsations
No engorged veins and scars
Apical impulse not visible
Palpation:
Apex beat present over the left 5th intercostal space 1cm medial to midclavicular line
No parasternal heave
No precordial thrill
No dilated veins
Auscultation:
S1 S2 heard ,No murmurs
RESPIRATORY EXAMINATION:
Upper respiratory tract - normal
Lower respiratory tract-
Inspection:
Chest bilaterally symmetrical,
Shape- elliptical
Trachea- Central
Palpation:
Trachea is Central
Normal chest movements
Vocal fremitus is normal in all areas
Percussion: in sitting postion
Rt. Lt
Supraclavicular. N(resonant). N
Infraclavicular. N N
Mammary region. N. N
Inframammary region. N. N
Axillary region. N. N
Infra axillary region. N. N
Supra scapular region. N. N
Interscapular region. N. N.
Infrascapular region. N. N
Auscultation:
Normal vesicular breath sounds
No added sounds
Vocal resonance is normal in all areas.
CNS EXAMINATION:
Higher motor functions - intact
Cranial nerves - intact
Motor system:
Rt- UL. LL. Lt- UL. LL
Bulk - normal N. N. N
Tone - N. N. N. N
Power - 5/5. 5/5. 5/5. 5/5
Reflexes:
UL LL
Biceps. 2+. 2+
Triceps. 2+. 2+
Supinator. 2+. 2+
Knee 2+. 2+
Ankle. 2+. 2+
Sensory system: intact
Co ordination is present
Gait is normal
No Cerebellar signs
No signs of meningeal irritation
INVESTIGATIONS:
SERUM CREATININE ON 16/11/23:
ASCITIC FLUID PROTEIN SUGAR ON 16/11/23:
ASCITIC FLUID AMYLASE ON 16/11/23:
ASCITIC FLUID FOR LDH ON 16/11/23:
SAAG ON 16/11/23:
CELL COUNT OF ASCITIC FLUID ON 17/11/23:
CUE ON 18/11/23:
CUE ON 23/11/23:
URINARY SAMPLE AS ON 8/12/23:
REPORT OF URINARY SAMPLE SENT ON 8/12/2023:
Early morning same was asked to be repeated by pathology pg's
Early morning sample report sent on 9/12/2023 and report showed:
Report of PT and INR :
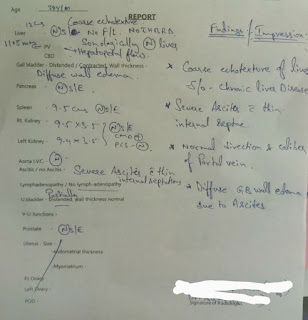
USG REPORT AS DONE ON 9/12/2023:
Urine culture report:
URINARY SAMPLE ON 12/12/2023:
UROLOGY REFERRAL WAS TAKEN I/V/O HAEMATURIA AND INTERNAL ECHOS IN THE BLADDER:
Uroflowmetry was done on 13/12/2023:
Urine culture report showed negative
REPEAT CUE REPORT:
URINE SAMPLE ON 15/12/2023:
CUE REPORT OF THE ABOVE SAMPLE:
URINE SAMPLE ON 17/12/2023:
CUE of the above sample:

24HR URINARY PROTEIN AND CREATININE REPORT:
Later Renal biopsy was done on 22/12/2023
COURSE IN THE HOSPITAL:39 YEAR OLD MALE CAR DRIVER BY OCCUPATION RESIDENT OF WEST BENGAL PRESENTED TO GM OPD WITH ABDOMINAL DISTENTION AND B/L PEDAL EDEMA SINCE 2 MONTHS.AFTER THOROUGH CLINICAL EVALUATION AND INVESTIGATIONS
DIAGNOSED AS CHRONIC LIVER DISEASE AND DIAGNOSTIC TAP SHOWED HIGH SAAG LOW
PROTEIN FOLLOWED BY THERAPEUTIC TAP AND PATIENT IMPROVED SYMPTOMATICALLY.HE THEN DEVELOPED CLOUDY TURBID AND HIGH COLOURED URINE
FOR WHICH UROLOGY REFERAL WAS DONE ON 12/12/23 AND X-RAY KUB AND UROFLOWMETRY WAS DONE WHICH WERE FOUND OUT TO BE NORMAL RULING OUT
BLADDER CALCULUS AND STRICTURE URETHRA.LATER 24HR URINARY PROTEIN VALUE SHOWED 3,834 MG/DAY AND 24 HR URINARY CREATININE SHOWED A VALUE OF
2.6GM/DAY.PATIENT IS SUSPECTED TO HAVE NEPHROTIC SYNDROME,TO CONFIRM THE DIAGNOSIS RENAL BIOPSY WAS DONE ON 22/12/23 AND PATIENT IS BEING DISCHARGED IN HAEMODYNAMICALLY STABLE CONDITION AND REVIEW TO GENERAL MEDICINE OPD WITH RENAL BIOPSY AFTER 10 DAYS.





RENAL BIOPSY REPORT:
PAJR LINK:
https://chat.whatsapp.com/ITRPEf7cMvU5FKyq5WtQaF














































Comments
Post a Comment